Where we are
Many factors influence public health statistics, and one that I have frequently mentioned is global migration. In December 2018, on Mexican national radio, I was invited to speak about the health implications of the new migrant caravans from Central America. Among the many consequences I mentioned, the most pressing was the possibility of a pandemic with migratory origins.
Approximately one year later, in December 2019, the first case of SARS-CoV-2 was reported in Wuhan, China. Four months later, the entire world was effectively shut down. We witnessed how a pandemic, exacerbated partly by global migratory flows and mobility patterns, paralyzed the globe.
The vulnerabilities in our data, patient management, and overall quality of care worldwide were revealed in full force, and global health systems were brought to their knees—not because the virus itself had a uniquely devastating impact on human health, but because the policies that resulted from it caused nearly irreversible damage.
There was a severe lack of coordination between experts on the matter and those responsible for delivering official messaging. However, this issue serves as a significant distraction. In reality, global healthcare systems and the public health initiatives of the last century have effectively controlled the mass spread of deadly infectious diseases.
Yet, determining the current state of health is challenging, and, frankly, some of the data don’t make much sense.
Infectious disease is not as significant a threat as it is sometimes portrayed to be. What we learned from "The COVID Operation" is that the level of panic far exceeded the actual risk posed by the disease itself. This trend is historically reflected as well. What we can see from the available data is that infectious and communicable disease outcomes have significantly improved over the past 35 years globally, although there has been a slight increase in the past four years.
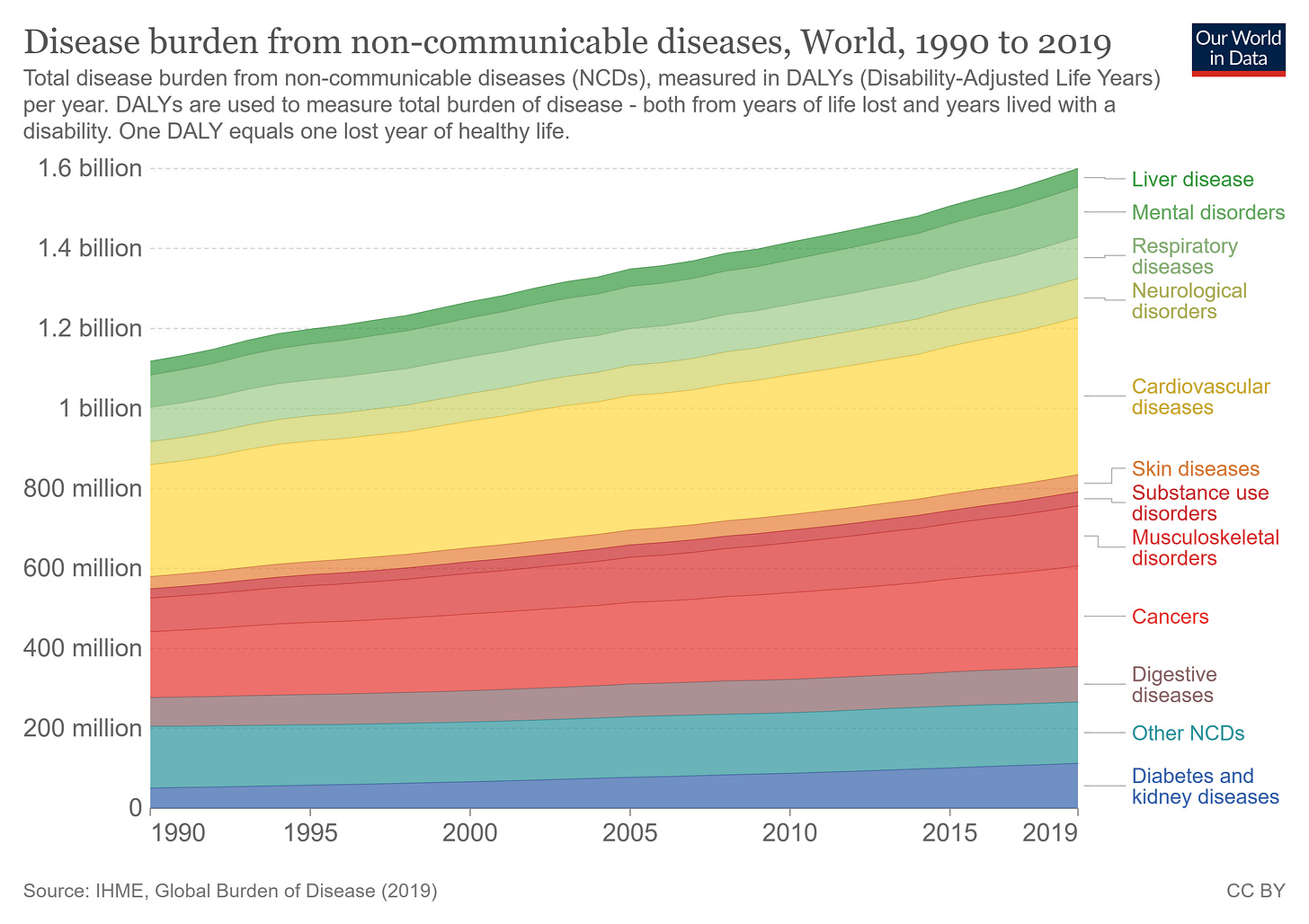
Interestingly, however, non-communicable disease (NCD) rates have risen at a nearly identical pace to the rise in infectious diseases during the same period. Specifically, chronic degenerative diseases, cancers, and similar NCDs have increased dramatically.
Why is this the case?
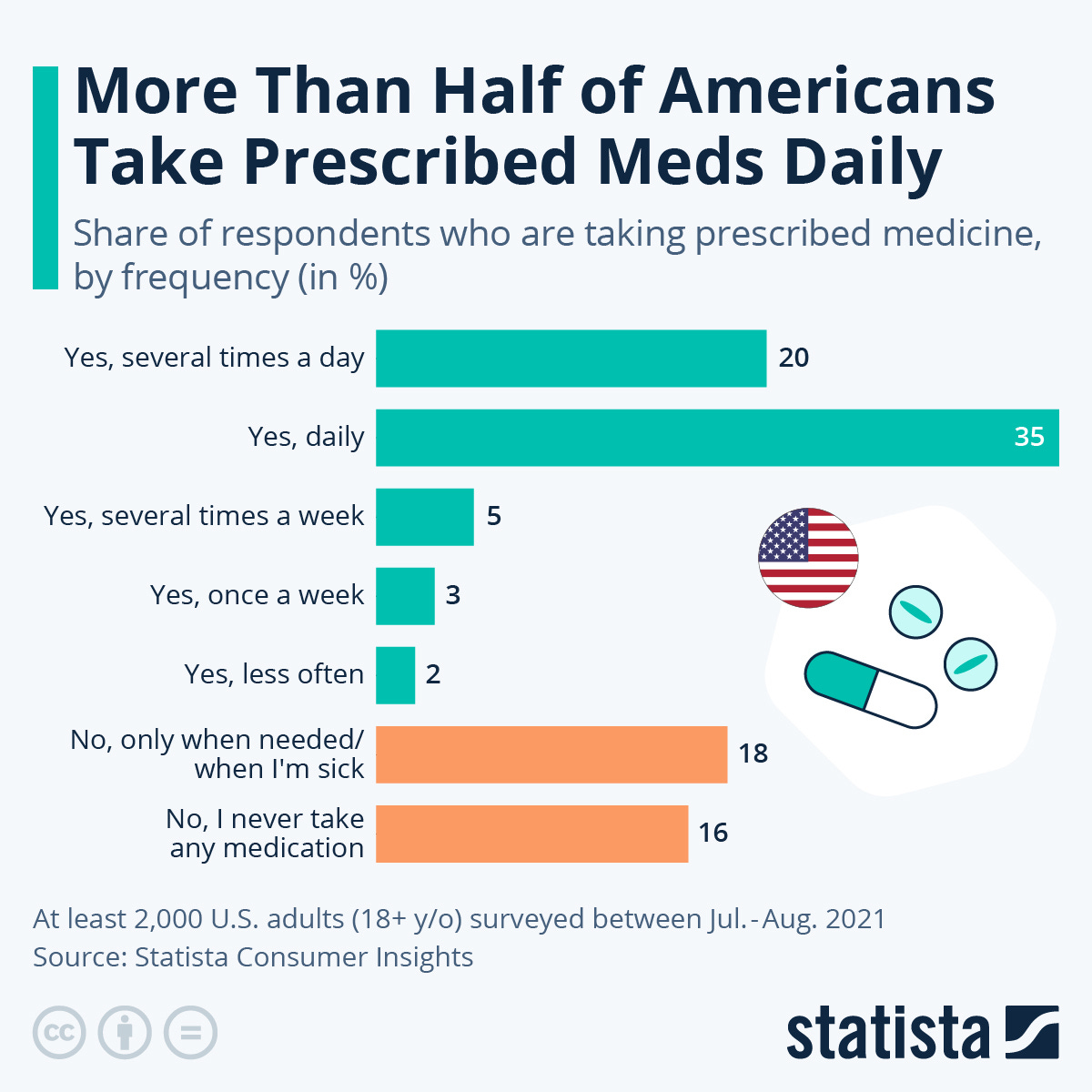
How is it possible that non-communicable disease rates are rising so dramatically when, in countries like the United States, more than half of Americans take prescription medications daily? What is the purpose of this constant ingestion of pharmaceuticals if patients continue to experience such poor health?
The reality is that we have a global “sick-care” system in place. Modern medicine has effectively reduced doctors to serial prescribers. Instead of addressing the root causes of diseases, we as clinicians have been trained to treat only the symptoms.
I believe there are various reasons for this. Not all the blame lies with doctors. The administrative burdens of private practice, patient oversaturation in healthcare systems, and, of course, the long-standing indoctrination of medical training in academia all contribute.
We are overridden by disease in our societies. Ballooning obesity rates, life expectancy rates stagnating…
…for the first time in nearly 60 years, global life expectancy dropped in 2020. Between 2010 and 2021, global life expectancy rose by only one year, compared to the 3.6-year increase in the preceding decade from 2000 to 2010.
Where we are going
Post-COVID Operation, these statistics on rising non-communicable and chronic disease appear to have worsened. As an expert in allergy and immunology, I often refer to statistics like those I mentioned in my Vital Signs post last week...
…how the market for antihistamines, which is the most popular remedial treatment for allergies (a non-communicable disease), is expected to more than double in size over the next 8 years, from $243 billion USD to nearly $650 billion USD. Why are these models consistently predicting a steep rise in these types of ailments?
Currently, patient care tends to focus solely on treating symptoms, ignoring underlying causes. For example: the GLP-1 revolution occurring in the United States, diabetes drugs are being repurposed as weight loss treatment. Why are we not more concerned as doctors in improving dietary/exercise habits than in feeding patients with drugs that are only remedial, and have shown to have serious side effects?
These sentiments are becoming more prevalent in the public discourse. Experts are starting to refer to the importance of health not only individual but that of populations as a whole. It’s starting to be reflected in certain policy proposals globally. This is precisely why our mission is so pivotal. We must go to those who have real power in shaping public health discourse and policy. The promotion of Biopolitikal Policy will be vital in determining the global health outcomes of the next decades.
Health is and will continue to be the most relevant issue for the next decades. As disease rates continue to rise into the future, we must do our best to stop this vicious cycle and provide patients with the care they deserve. As patients further understand how detrimental this current system is, they will begin to look for care alternatives. This will force providers and health systems to adjust their approach.
I predict integrative medicine will be more prevalent. Personalized, precision medicine. Focusing on the root causes of illness rather than solely addressing symptoms. Functional medicine considers the individual's unique genetic, biochemical, and lifestyle factors, offering a more comprehensive understanding of health.
This isn’t some far-off vision of the future. These alternatives exist today.
I think in many aspects we are heading in the right direction. Technological advancements in medicine are easing the workloads of many physicians. AI tools are innovating clinical workflows and allowing providers to streamline their processes, reducing administrative costs. This is true also for drug manufacturing and drug delivery systems. Making these systems more efficient will cut costs of production, and in the long term translate into lower cost of care for patients.
As functional medicine gains traction, we should expect pharmaceuticals to increasingly collaborate with practitioners in this field, resulting in more effective and patient-centric interventions. Collaboration from every sector of society will be necessary in navigating this changing landscape of global health.
FIN